Depression or Nervous System Fatigue?
- Rebecca Rinnert
- 4 days ago
- 5 min read

How Chronic Stress Dysregulates the Body and What Helps Restore Balance
January arrives quietly, yet for many people it feels heavy. Motivation is low. Energy is thin. Sleep doesn’t restore. Even after rest, something feels off.Many begin to wonder: Is this depression? Or am I just exhausted beyond words?
For a growing number of people, the answer lies not in a mood disorder, but in nervous system dysregulation caused by chronic stress fatigue. When the body has spent too long in survival mode, exhaustion becomes physiological, not psychological.
This article explores the difference between depression and nervous system fatigue, the signs of trauma-related exhaustion, and somatic, nervous-system-friendly strategies that support real regulation rather than pushing through.
Why Exhaustion Peaks in January
January is often when the body finally stops running.
After months or years of chronic stress, many nervous systems stay mobilized through sheer necessity. Work pressure, emotional strain, relational stress, health issues, caregiving, uncertainty. The system adapts by staying alert, productive, and functional.
When external demands slow down, the nervous system no longer needs to override exhaustion. What follows is often a delayed stress response: collapse, fatigue, fog, emotional flatness.
From a nervous system perspective, this is not weakness. It is a protective downshift.
Seasonal darkness, reduced movement, and post-holiday letdown can amplify this state, especially for people with a history of trauma or long-term stress.
Depression vs Nervous System Fatigue: Key Differences
Although symptoms may overlap, depression and nervous system fatigue are not the same. Confusing the two can lead to treatments that miss the root cause.
Depression often involves:
Persistent low mood or hopelessness
Loss of pleasure or interest
Negative self-concept or guilt
Reduced motivation tied to mood
Symptoms relatively stable across contexts
Nervous system fatigue often involves:
Profound physical exhaustion
Feeling “shut down,” numb, or foggy
Low motivation due to depleted energy, not despair
Moments of clarity or aliveness when safety increases
Symptoms that fluctuate with stress, rest, and relational context
Many people with chronic stress fatigue still want to engage with life. Their system simply does not have the capacity.
This distinction matters. You cannot think your way out of a depleted nervous system.

Signs of Nervous System Dysregulation and Chronic Stress Fatigue
Nervous system dysregulation shows up across body, mind, and relationships.
Physical signs
Persistent fatigue not relieved by sleep
Heavy limbs, slowed movement
Tension or collapse in posture
Digestive issues, headaches, immune vulnerability
Feeling cold, flat, or low-energy
Emotional signs
Emotional numbness or blunting
Irritability without clear cause
Reduced emotional range
Feeling disconnected from joy or desire
Cognitive signs
Brain fog
Reduced concentration
Forgetfulness
Difficulty making decisions
Relational and behavioral signs
Social withdrawal without wanting to isolate
Reduced tolerance for stimulation
Avoidance of demands
Functioning at a minimum, not from laziness but conservation
Many of these reflect a freeze or functional shutdown response, a common trauma-related survival state.
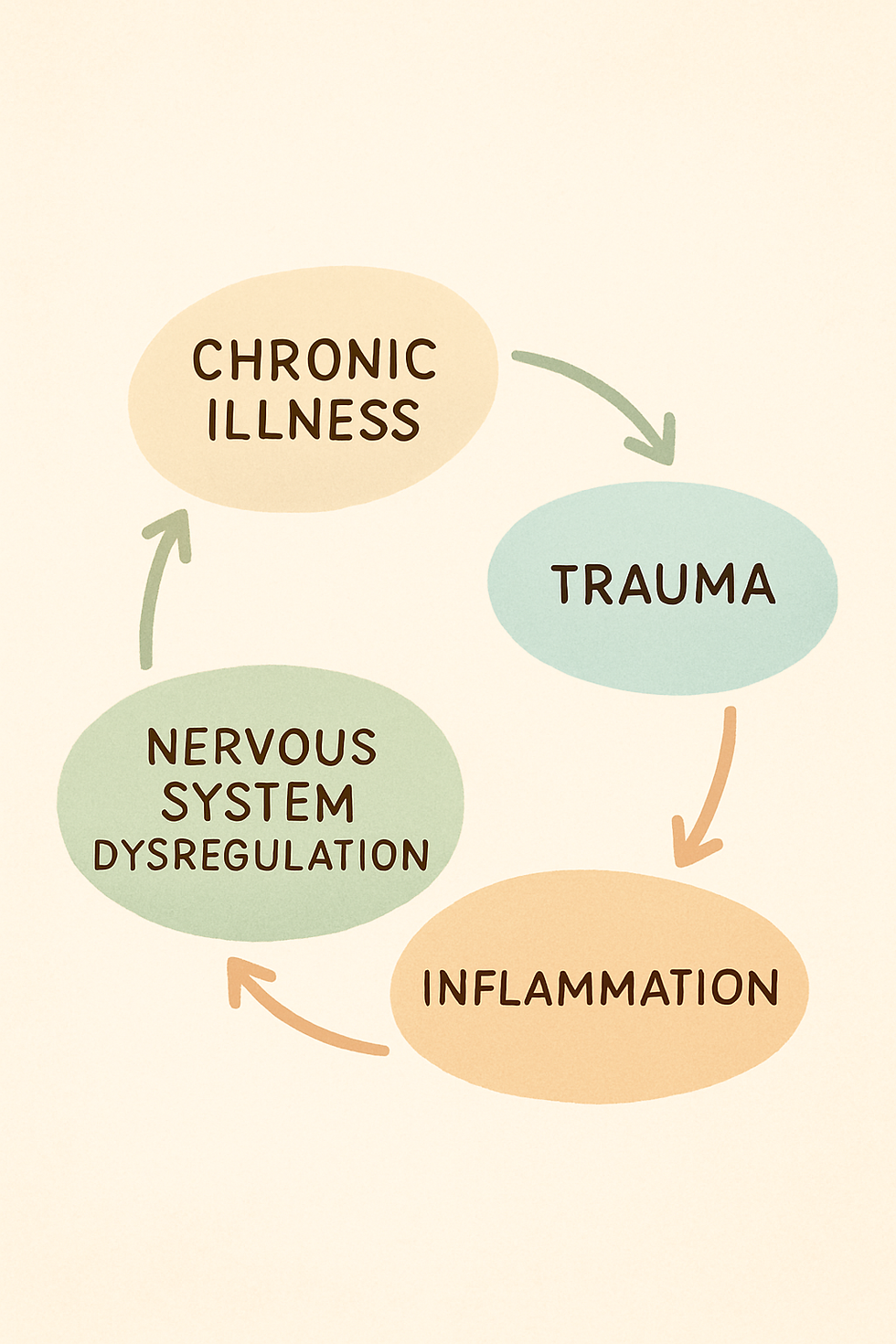
Trauma and Fatigue: How Long-Term Stress Depletes the Nervous System
Trauma is not only defined by extreme events. Ongoing emotional strain, relational unsafety, chronic pressure, medical stress, or repeated boundary violations all shape the nervous system.
Over time, the body learns that activation is dangerous or unsustainable. Instead of fight or flight, it shifts toward conservation.
This is where trauma and fatigue meet.
The nervous system prioritizes survival over vitality. Energy is preserved. Non-essential functions are dialed down. This is not a disorder. It is adaptation.
Why Rest Alone Often Doesn’t Help
Many people try to fix exhaustion with sleep, time off, or wellness routines, only to feel frustrated when nothing changes.
The reason is simple:A dysregulated nervous system does not respond to rest the same way a regulated one does.
Without felt safety, rest can even increase discomfort. Slowing down may bring awareness to sensations the system learned to suppress.
What’s needed is not more rest, but a somatic nervous system reset.
Somatic, Nervous-System-Friendly Strategies to Restore Regulation
Somatic approaches work with the body’s rhythms rather than forcing change.
1. Orienting to safety
Gently noticing your environment: light, colors, sounds, supportive surfaces. This signals the nervous system that the present moment is not threatening.
2. Micro-regulation instead of big practices
Short moments of grounding throughout the day are more effective than long sessions. Think seconds, not minutes.
3. Supporting regulation without forcing breath
For some systems, breathing exercises increase activation. Instead, notice the natural breath or place a hand on the body without changing anything.
4. Titration and pacing
Healing happens in small doses. Overdoing “self-care” can recreate stress. Less is often more.
5. Reconnecting with bodily signals
Noticing hunger, warmth, fatigue, or comfort rebuilds trust between body and mind.
These strategies help the nervous system remember how to move between activation and rest safely.
When to Seek Professional Support
If exhaustion persists, support matters.
Trauma-informed therapy, somatic approaches, or nervous system–based interventions can help restore regulation gently. Medical evaluation is also important to rule out physical causes.
The goal is not to label, but to listen to what the system is communicating.
Exhaustion Is Not a Failure
Chronic stress fatigue is not a lack of resilience. It is often the result of too much resilience for too long.
The body does not need discipline. It needs safety, pacing, and attunement.
Healing begins not by pushing harder, but by allowing the nervous system to soften its grip on survival.
Frequently Asked Questions About Nervous System Fatigue
Can nervous system dysregulation feel like depression?
Yes. Nervous system dysregulation can closely resemble depression, including fatigue, numbness, and low motivation. The key difference is that in nervous system fatigue, symptoms often improve when safety, rest, or regulation increases, whereas depression tends to be more persistent and mood-based.
How do I know if I’m exhausted from stress or actually depressed?
If you still want connection, creativity, or engagement but feel physically unable to access energy, this often points to chronic stress fatigue rather than depression. A trauma-informed professional can help differentiate the two.
Why am I tired all the time even though I sleep enough?
Chronic stress keeps the nervous system dysregulated, preventing deep restoration. Sleep alone cannot reset a nervous system that remains in survival mode during waking hours.
Can trauma cause long-term fatigue?
Yes. Trauma and fatigue are closely linked. Long-term or unresolved trauma can lead to nervous system shutdown, reduced energy, and chronic exhaustion as a protective response.
What is a somatic nervous system reset?
A somatic nervous system reset involves gentle, body-based practices that help the nervous system return to regulation by increasing safety, awareness, and capacity, rather than forcing relaxation or productivity.
Do breathing exercises help with nervous system dysregulation?
They can, but not always. For some people with trauma, controlled breathing can increase activation. Somatic approaches emphasize choice, pacing, and noticing rather than forcing breath changes.
When should I seek professional help for exhaustion?
If fatigue persists for weeks or months, impacts daily functioning, or is accompanied by shutdown, numbness, or anxiety, professional trauma-informed or medical support is recommended.


Comments