Chronic Illness & the Nervous System: Why Your Body’s Flooded—and How to Find Calm
- Rebecca Rinnert
- Dec 2, 2025
- 4 min read
Living with chronic illness can feel like your body is constantly sounding an alarm—fatigue, inflammation, flare-ups, pain, brain fog, emotional overwhelm, and a sense that something deeper is going on beneath the surface. Many people with autoimmune diseases, long COVID, chronic fatigue, and complex pain disorders intuitively feel there is a connection between their symptoms and the stress or trauma they’ve lived through. Yet they’re often dismissed with explanations like “it’s just stress” or “your labs are fine.” But there is a connection—and the science is becoming clearer every year.This article explains why chronic illness trauma and nervous system dysregulation so often overlap, why your body may feel “flooded,” and how gentle somatic healing practices can begin to restore regulation and safety.
What Chronic Illness Does to Your Nervous System
Chronic illness places the nervous system into a state of near-constant vigilance. When your immune system is overactive, your body interprets it as a threat. When your energy system is depleted or dysregulated, the body interprets that as a threat too.
Many people with chronic illness trauma describe feeling stuck between exhaustion and hyper-alertness—tired but wired, overwhelmed yet unable to rest.
Fatigue, inflammation, and brain fog explained
Fatigue often stems from the body running in “survival mode” for too long.
Inflammation can increase sympathetic activation and pain-sensitive pathways.
Brain fog often appears when the prefrontal cortex goes offline in response to chronic threat signals.
From a polyvagal perspective, this is the body protecting you—not failing you.
Fight/flight/freeze patterns in chronic illness
Because of the chronic illness and stress connection, you may experience:
Fight: tension, irritability, inflammation spikes
Flight: anxiety, restlessness, difficulty resting
Freeze: exhaustion, collapse, shutdown, brain fog
Fawn: people-pleasing that worsens depletion
These responses are not “psychological problems.”They are physiology—and they make complete sense in the context of chronic illness trauma.

The Trauma–Autoimmune Link: What Science Reveals
The trauma autoimmune link is one of the most rapidly growing areas of research. Multiple studies now suggest that trauma—particularly early-life or chronic trauma—can reshape immune function for decades.
Key findings include:
Traumatised nervous systems produce more inflammatory cytokines.
Chronic hypervigilance affects the vagus nerve’s anti-inflammatory pathways.
ACEs (Adverse Childhood Experiences) significantly increase the risk of autoimmune illness later in life.
People with chronic illness trauma are more likely to experience flare-ups during periods of heightened emotional stress.
This doesn’t mean trauma causes illness—but it can prime the body to respond differently to stress, infection, and inflammation.
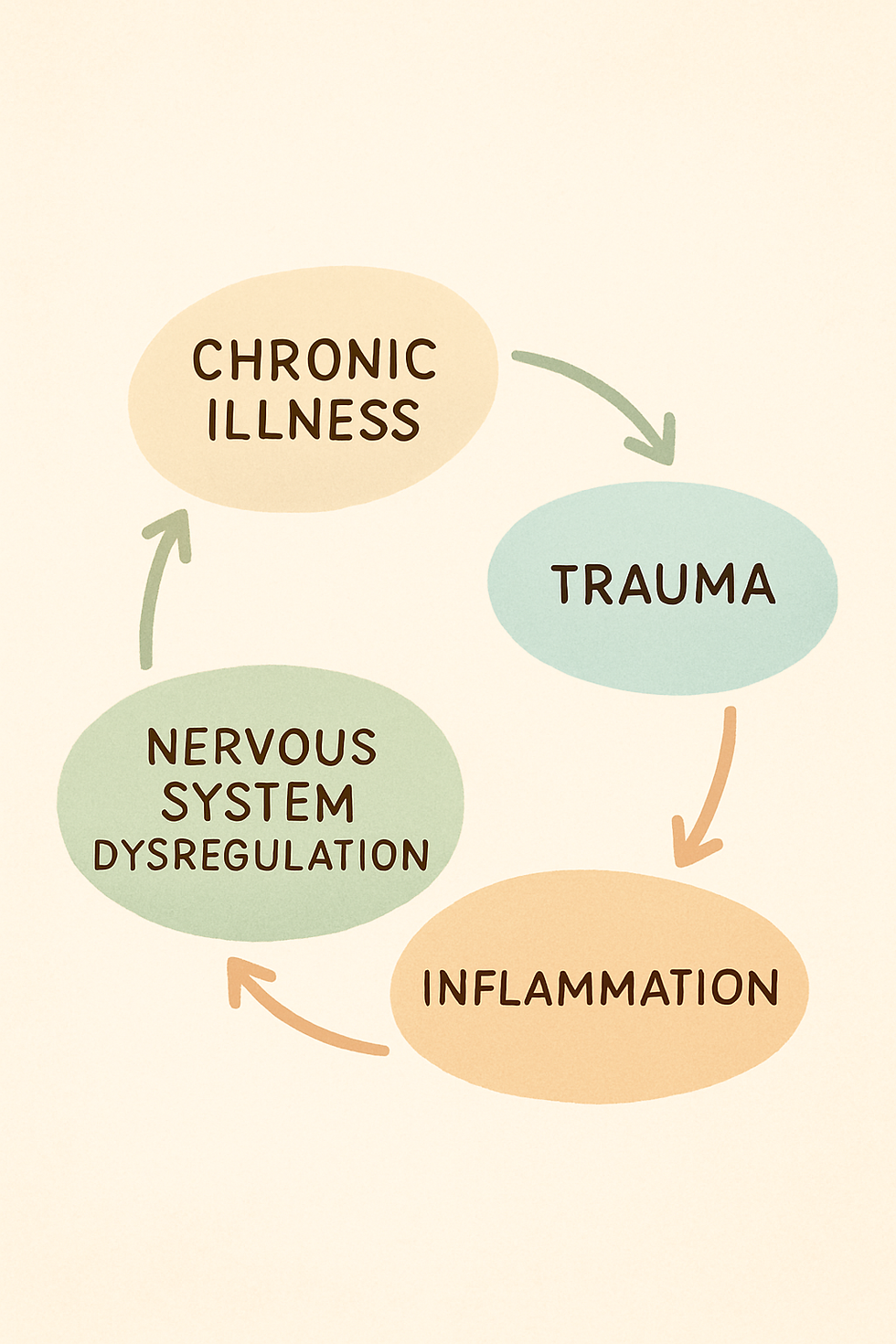
Trauma, immune dysregulation, and nervous system dysregulation form a feedback loop that keeps the body in survival mode.
Why Your Body Feels “Flooded”: The Physiology of Dysregulation
When your nervous system has been under pressure for a long time—through illness, stress, or trauma—it becomes more sensitive to internal cues. Pain, fatigue, and inflammation feel louder. Minor triggers feel bigger. Ordinary tasks feel overwhelming.
Think of dysregulation like a flooded engine:your body is trying to run, but there’s too much activation in the system to function smoothly.
Signs of a “flooded” system:
feeling overwhelmed for no obvious reason
flare-ups after small stressors
sudden exhaustion or shutdown
difficulty digesting food
sensitivity to light, noise, or touch
feeling disconnected or spacey
chronic inflammation spikes
This is not “mental weakness” or “being dramatic.”It’s a biological survival response.
This is where polyvagal theory chronic illness research offers insight: when the vagus nerve remains inhibited, the body cannot shift into rest, repair, digestion, or healing.
Somatic Healing Tools to Calm a Dysregulated Nervous System
Healing chronic illness trauma isn’t about ignoring symptoms—it’s about teaching your nervous system that it’s allowed to feel safe again.
Below are gentle, realistic tools that meet the body where it is.
Gentle daily regulation practices
1. Breathwork for safety, not performance
Try soft, slow, non-forceful exhalations.Example: Inhale for 4, exhale for 6—only if it feels good.
The goal is downshifting, not perfect breathing.
2. Grounding through contact points
Place your hands on your legs, lean into a chair, or feel your feet against the floor.Let your body register, “I am supported.”
3. Orienting: help your body exit survival mode
Look around the room slowly. Let your eyes land on something pleasant or neutral.This signals to the brainstem: “There is no immediate threat.”
4. Vagal toning through gentle sound
Humming, soft singing, or long “mmm” sounds can stimulate the vagus nerve in a safe, simple way.
5. Micro-movements to release tension
Small, slow, barely noticeable movements help reduce freeze-based stiffness:
rolling shoulders
small spinal sway
gentle rocking
stretching your toes
These somatic healing chronic illness practices work best when done consistently in tiny doses—especially for trauma and chronic fatigue.
When Chronic Illness Trauma Needs Professional Support
Consider reaching out for help if you experience:
frequent shutdown, panic, or dissociation
difficulty managing daily life
symptoms that worsen with emotional stress
a history of trauma that hasn’t been processed
chronic illness trauma patterns that feel overwhelming
Trauma-informed therapy, somatic experiencing, neurobiologically grounded coaching, and mind-body medicine can be powerful support systems.
Working with someone who understands both trauma and chronic illness can reduce shame and help you move toward safety and regulation at your own pace.
Conclusion: Your Body Isn’t Broken—It’s Trying to Protect You
If you live with chronic illness trauma, long COVID, autoimmune disease, or chronic fatigue, your symptoms are not signs of weakness—they are signs of a nervous system trying to navigate immense pressure.
Your body isn’t failing.Your body is communicating.Your body is protecting you.
And with the right support, awareness, and gentle somatic practices, your system can learn that it’s safe to soften, rest, and heal.
You deserve that safety.
FAQ
1. Is chronic illness trauma “all in my head”?
Not at all. Trauma and dysregulation affect immune, hormonal, and inflammatory systems. The effects are deeply physical.
2. Can somatic practices cure chronic illness?
They don’t cure illness, but they support regulation, decrease flare-ups, and reduce symptom intensity.
3. Why do stress and emotions trigger my symptoms?
Because nervous system dysregulation can amplify pain, inflammation, and fatigue. Your body reacts more strongly to internal and external cues.
4. Is the trauma–autoimmune link scientifically supported?
Yes. Studies on ACEs, neuroimmune pathways, and inflammation show strong correlations between trauma and autoimmune risk.
5. How long does healing take?
Every body is different. Progress comes from consistent, gentle work—not force.



Comments